Medical Face Mask Standards and Regulations
Specifications developed by the American Society of Testing and Materials (ASTM) are referenced by the FDA as the required standard in the USA. The current standard ASTM F2100-11 (2011) specifies the performance requirements for Medical Face Masks with five basic criteria:
1. BFE (bacterial filtration efficiency) measures how well the mask filters out bacteria when challenged with an bacteria-containing aerosol. ASTM specifies testing with a droplet size of 3.0 microns containing Staph. aureus (average size 0.6-0.8 microns). In order to be called a medical/surgical mask, a minimum 95% filtration rate is required. Moderate and high protection masks have bacterial filtration rates of 98% to greater than 99%.
Some manufacturers use the Modified Greene & Vesley method to determine the BFE rating. This method is NOT recommended by ASTM for product comparison or evaluating consistency.
2. PFE (particulate filtration efficiency) measures how well a mask filters sub-micron particles with the expectation that viruses will be filtered in a similar manner. The higher the percentage, the better the mask efficiency. Although testing is available using a particle size from 0.1 to 5.0 microns, ASTM F2100-11 specifies that a particle size of 0.1 micron be used. When comparing test results it is important to note the size of the test particles used, as use of a larger particle size will produce a misleading PFE rating.
3. Fluid Resistance reflects the mask’s ability to minimize the amount of fluid that could transfer from the outer layers through to the inner layer as the result of a splash or spray. ASTM specifies testing with synthetic blood at pressures of 80, 120, or 160 mm Hg to qualify for low, medium, or high fluid resistance. These pressures correlate to blood pressure: 80 mm Hg = venous pressure, 120 mm Hg = arterial pressure, and 160 mm Hg correlates to potential high pressures that may occur during trauma, or surgeries that include high pressure irrigation such as orthopedic procedures.
4. Delta P (pressure differential) measures the air flow resistance of the mask and is an objective measure of breathability. A controlled flow of air is driven through a mask and the pressure on either side of the mask is determined. The difference in pressure is measured and divided by the surface area (cm2) of the mask segment tested. The higher the Delta P value, the harder it is for the wearer to breathe. The Delta P is measured in units of mm H2O/cm2. The ASTM standard requires that masks have a Delta P of less than 5.0, as a higher value would be considered too “hot” for general medical or surgical use. Masks with a Delta P of less than 4.0 are considered acceptable, while masks with a Delta P less than 2.0 would be considered “cool”.
5. Flame Spread: Operating rooms contain sources of oxygen and other gases used for anesthesia, and there are potential fire hazards from electrosurgical procedures such as lasers or cautery equipment. All products used within the operating room, including face masks, are tested for flame resistance. As part of ASTM F2100 testing, masks must withstand exposure to a burning flame (within a specified distance) for three seconds.
In addition to the above tests, all face masks must be tested to an international standard (ISO 10993-5, 10) for skin sensitivity and cytotoxic tests to ensure that no materials are harmful to the wearer. Tests are conducted on materials used in construction of the mask which come in contact with the user's skin.
Table II: Summary of ASTM Standards
|
ASTM F2100-11 (2011) REQUIREMENTS
FOR MEDICAL FACE MASKS
|
|
Test:
|
Low
Barrier
|
Moderate
Barrier
|
High
Barrier
|
|
BFE (Bacterial Filtration Efficiency)
at 3.0 micron ASTM F2101
|
≥ 95%
|
≥ 98%
|
≥ 98%
|
|
PFE (Particulate Filtration Efficiency)
at 0.1 micron ASTM F2299
|
≥ 95%
|
≥ 98%
|
≥ 98%
|
|
Delta P (Differential Pressure)
MIL-M-36954C, mm H2O/cm2
|
< 4.0
|
< 5.0
|
< 5.0
|
|
Fluid Resistance to synthetic blood
ASTM 1862, mm Hg
|
80
|
120
|
160
|
|
Flame Spread
16 CFR part 1610
|
Class 1
|
Class 1
|
Class 1
|
Frequently Asked Questions
What is the purpose of a Medical Face Mask?
In the Operating Room (OR), surgical masks protect the sterile field from possible contamination, primarily as a result of coughing, sneezing or talking. A mask may also protect clinicians from the byproducts of surgical procedures such as bone chips, splashes of body fluids, and smoke plume resulting from laser or electrosurgical techniques.
Outside of the OR masks are used for standard precautions to protect clinicians and patients from pathogens that may spread by blood or other body fluids, secretions or excretions. Surgical and procedure masks are effective against droplet transmission.
What is the difference between a surgical mask and a procedure mask?
A surgical mask is used inside the operating room or during other sterile procedure areas to protect the patient environment from contamination. It also protects the clinician from contaminated fluid or debris generated during the procedure. Surgical masks have ties so that they can be adjusted for fit, and are tied over top of a surgical or bouffant cap.
A procedure mask is used for performing patient procedures, or when patients are in isolation to protect them from potential contaminants. They are used to protect both patients and staff from the transfer of respiratory secretions or other fluids or debris. They are used for ‘respiratory etiquette’ to prevent people from spreading germs via talking, coughing, or sneezing. Procedure masks have ear loops for quick donning, and since they do not slide on the hair can be worn without a surgical cap.
How long is my face mask effective?
The filtration efficiency and protective ability of a face mask is compromised when the mask becomes wet, torn or dislodged. Generally speaking, the higher protection value of a mask the longer it will maintain filtration, however there is no set rule for how long a mask should be worn as it depends on humidity levels, respiration rate, nasal discharge, talking, etc. A mask should be worn for only one patient procedure or visit. If a mask gets wet or soiled it should be replaced.
Why is the fit of a mask important?
A mask is only as effective as its fit. There should be no gaps along the side, around the nose or under the chin that would allow air and droplets to bypass the filter medium. The mask should always be properly adjusted to fully cover both the mouth and nose. A well-fitting mask stays in place over the nose and cheeks and even a regular mask will prevent fogging of eyeglasses if it fits properly. Masks should not be worn underneath the nose or dangling around the neck – they should either be fully on, or disposed of.
How do I ensure a good fit?
There are several things that contribute to a good fit. The most important consideration is the nose piece. It should mold over the nose and cheeks and maintain its shape over time. It should not kink or break when adjusted. Individuals with wider faces should select a mask that ensures full coverage over the face and under the chin. The upper tie should sit at the crown of the head, and the lower tie should be tied behind the neck to hold the sides of the mask against the face to prevent any gaping.
How do I know that the mask is on correctly?
1. The metal nose piece is at the top
2. The white, or smoothest side, is on the inside against the wearer’s skin; the color always faces out
3. The pleats fall downwards and away from the nose (called a “waterfall” pleat)
What tests or ratings should I rely on to ensure my mask is safe?
Specifications developed by the American Society of Testing and Materials (ASTM) are generally accepted as the industry standard. Beware of mask ratings that do not follow ASTM guidelines. Some manufacturers may refer to “filtration rates” or the “number of layers” as an indication of effectiveness. These vendors may not be adhering to the ASTM standards and should be questioned for specific test data.
What else should I know about face masks?
All individuals using face masks must be aware of the protective capabilities of the mask being worn. Health care workers should assess their risk of exposure to blood, body fluids, excretions, and other potential hazards; and choose their mask accordingly.
A face mask is considered to be contaminated once it has been used, and should be discarded immediately. A mask should be removed by the edges or the ties rather than the front panel.
As part of PPE (Personal Protective Equipment), masks with integrated visors are recommended to ensure compliance with eye protection. Protective apparel includes all equipment that prevents potentially infectious material from contaminating clothing, skin, eyes, mouth, nose, or other mucous membranes.
What is the difference between a medical mask and a respirator?
Medical masks (surgical/procedure masks) are loose fitting masks that cover the mouth and nose. They are designed to stop large droplets and splashes or sprays, but are not designed to seal tightly to the face or filter small airborne contaminants.
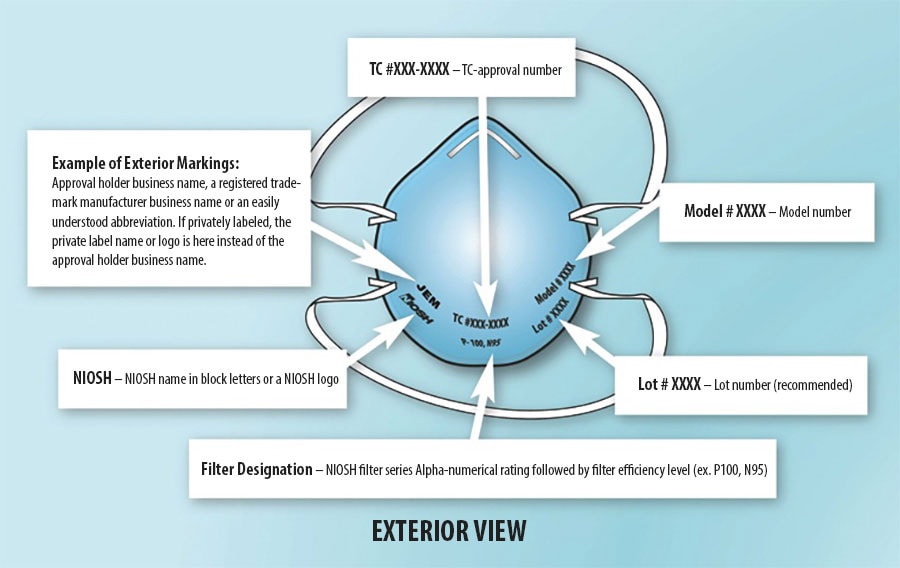
A respirator is an item of PPE designed to reduce exposure to airborne contaminants. Known airborne pathogens include TB, SARS, Anthrax, and Hanta virus. Respirators must be individually selected to fit the wearers face and shown to provide a good seal. They also must be certified by NIOSH, and used within a comprehensive respiratory program including fit testing and training.
|